Magnetic Balance: How TMS Steadies Bipolar Moods Without Medication’s Heavy Price
- Goodwin Health Cafe
- Jun 10, 2025
- 3 min read
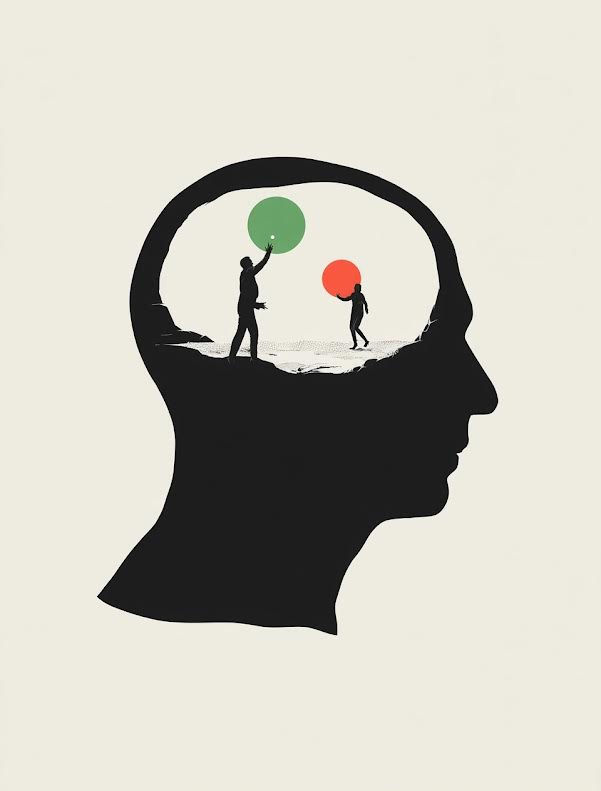
Living with bipolar disorder often feels like walking a tightrope stretched between crushing lows and dizzying highs. Medications such as mood stabilizers and atypical antipsychotics can keep that rope steady, yet their daily toll — weight gain, metabolic problems, tremors, and mental fog — pushes many people to skip doses or abandon treatment. Non-adherence fuels relapse, hospitalization, and needless suffering.
For a growing number of patients and clinicians, TMS for bipolar disorder is emerging as a new safety net. Transcranial magnetic stimulation (TMS) delivers focused magnetic pulses to specific brain circuits, aiming to lift bipolar depression and smooth mood swings without the whole-body side effects tied to pills.
Why Look Beyond Medication?
Medication remains the first-line approach for bipolar disorder, but real-world studies show discontinuation rates close to 50 percent within a single year. The top reasons include:
Metabolic complications such as rapid weight gain and elevated blood sugar or cholesterol
Cognitive dulling that slows thinking and memory
Sedation that undermines work or school performance
Hormonal changes that worry women of child-bearing age
Patients who stop medication are five times more likely to cycle into mania or suicidal depression. An alternative that stabilizes mood while preserving everyday functioning would fill a critical gap.
How TMS Works for Bipolar Disorder
A figure-eight coil rests gently on the scalp. Each magnetic pulse passes painlessly through bone and skin to generate a tiny electric current that nudges neurons in the dorsolateral prefrontal cortex toward healthier firing patterns. Over four to six weeks, five sessions per week, these “nudges” retrain mood circuits much like physiotherapy retrains injured muscles.
Benefit | What it means in practice |
No sedation | Patients can drive to appointments and resume normal activities immediately. |
Drug-free | No metabolic, endocrine, or cognitive burden. |
Focal action | Only the targeted brain network is stimulated, limiting unintended effects elsewhere. |
Adjustable | Clinicians fine-tune frequency, coil angle, and pattern if hypomanic symptoms appear. |
What the Evidence Shows
Response and remission
A 2023 systematic review and meta-analysis of TMS in bipolar depression reported that low-frequency right-sided and high-frequency left-sided protocols reduced depressive symptoms with effect sizes similar to unipolar depression. The review also found that treatment-emergent mania was exceedingly rare when clinicians followed standard safety guidelines.
Complementing those findings, a large real-world registry of more than 800 patients showed that outcomes for bipolar depression matched those for major depressive disorder after a full TMS course.
Professional endorsement
The American Psychiatric Association position statement on TMS affirms that properly delivered TMS is safe and effective for mood disorders and calls for broader insurance coverage so patients with bipolar depression can access evidence-based neuromodulation.
Safety Profile
Side effects are usually mild and short-lived:
Scalp discomfort or mild headache during or shortly after stimulation
Facial muscle twitching that stops once the coil is repositioned
Transient fatigue in some patients during the first few sessions
Serious events such as seizures are extremely rare (less than 0.1 percent). Careful screening and protocol adjustments also help prevent treatment-emergent mania. Patients with a recent hypomanic episode typically receive lower starting intensities or slightly different coil positions.
A Week-by-Week Treatment Roadmap
Consultation and mapping• A psychiatrist reviews diagnosis, medication history, and medical contraindications.• Motor threshold mapping sets personalized dosing.
Weeks 1–2: Building momentum• Twenty-minute sessions Monday through Friday.• Many patients notice subtle energy or concentration gains by the tenth session.
Weeks 3–4: Symptom lift• Mood scales such as the Montgomery-Åsberg Depression Rating Scale track progress.• Coil position or frequency is adjusted to maximize benefits.
Weeks 5–6: Consolidation• Residual depressive thoughts often fade.• Education on sleep, exercise, and relapse warning signs begins.
Post-course maintenance• Monthly booster sessions are offered if stress or seasonal change triggers mood dips.
Integrating TMS With Whole-Person Care
TMS is most powerful when paired with supportive measures:
Cognitive-behavioral therapy to strengthen new thought patterns
Regular aerobic exercise that boosts neuroplasticity via brain-derived neurotrophic factor (BDNF)
Balanced nutrition to support neurotransmitter synthesis and gut-brain health
For those who tolerate them, low-dose mood stabilizers may be reintroduced after TMS ends to maintain long-term equilibrium without heavy side effects.
Insurance and Access Tips
Document failure or intolerance of at least two mood stabilizers; most insurers require this proof.
Request a letter of medical necessity citing current guidelines and the APA endorsement.
Check out-of-network benefits if no local clinic offers bipolar-specific protocols. Goodwin Health Café assists with benefit verification and appeals, minimizing financial hurdles.
Medication saves many lives, but its side effects can also steal quality of life. TMS for bipolar disorder offers a focal, drug-free approach that relieves depressive episodes, preserves cognition, and keeps mania risk low. Backed by meta-analytic evidence and national psychiatric guidelines, TMS is no longer experimental. It is a bright, magnetic beam of hope for people who have struggled to balance mood stability and everyday vitality. If you or someone you love is seeking durable relief without medication’s heavy price, exploring TMS may be the next step on the journey to balanced living.






Comments